Changing lives and transforming organizations through leadership, education, and consultation
While most survivors of a mild traumatic brain injury (mTBI) keep a laser-like focus on the physical healing of the brain, one aspect of the therapeutic process is often an afterthought and usually forgotten and overlooked. That important aspect is a person’s psychological and emotional well-being.
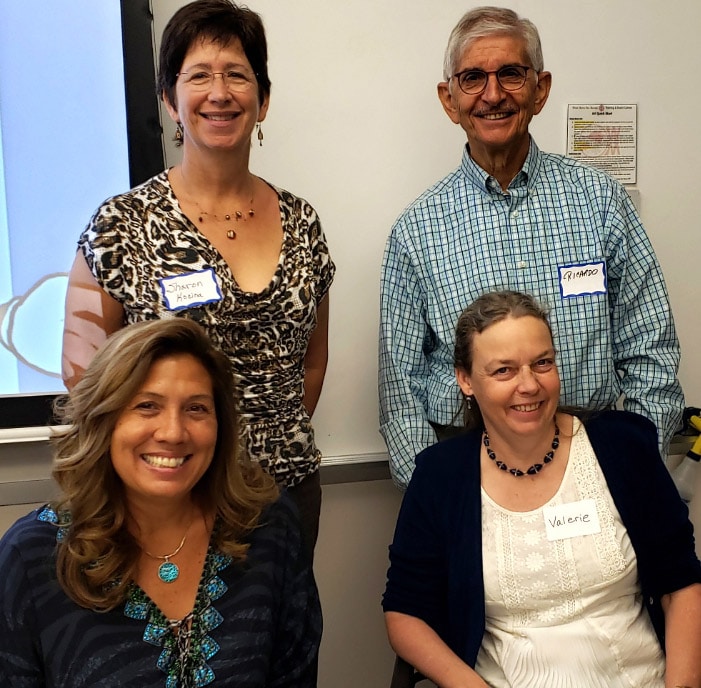
To help survivors and their families understand the importance of the mental side of recovery the Brain Injury Hope Foundation’s Survivor Series on September 13, 2019, featured a panel of experts at its “The Benefits of Counseling Following Traumatic Brain Injury” luncheon at the West Metro Fire and Rescue Training and Event Center in Lakewood, Colorado, facilitated by Board President and Executive Director, Gayann Brandenburg.
The following experts shared their insights:
Rita Coalson, MA, LPC, NCC
Psychotherapist (Grief Therapy, Trauma, Boundary Issues, Life Transitions)
Aloha Counseling Services
Email: ritacoalson@gmail.com
303-907-8973
Ricardo Esparza, Retired
Ph.D
P.O. Box 17145
Boulder, CO
303-447-1257
Sharon Kocina, MA, LPC
Helping You Go From Surviving to Thriving
303-444-2003
Email: Sharon@sharonkocina.com
https://sharonkocina.com
Valerie Stone, Ph.D., Psy-C
Licensed Psychologist Candidate
833-883-7527
Email: aboutbraininjury@live.com
“When you go to counseling you should expect to be in a safe space to be whom you are, where you
are,” Coalson said. “If you don’t have a safe space you will not open up. Interview your therapist so that
you can be you and trust that person.”
“Yes, a safe space is extremely important,” Stone said. “You should feel supported in being who you
want to be and be treated with respect.”
After finding the right therapist Kocina emphasized celebrating the little successes in your recovery.
“Look for changes, even if they are baby steps,” she said. “And take time to rest before and after your
appointments. You will need to have energy going into therapy.”
“And when you are in an appointment take notes and ask for handouts.”
“Having a patient write in a journal is extremely helpful,” Esparza noted as it is easier to go back and
chart your progress as you recover from a TBI. “And talk about a strategy.”
Part of that strategy includes having hope that you will get better and surrounding yourself with loving
and kind people, Esparza explained.
Another facet Esparza stressed is sharing your recovery with your spouse and family members as he
related a story of one gentleman who would not open up to his wife as he felt he was protecting his
spouse.
“It’s very, very important not to be stingy by hogging up the injury and not allowing someone to be
compassionate to you,” Esparza said. “This is a life-changing event, and it’s life changing for them, too.”
One of the first steps to mental recovery is a grieving process.
“Don’t be put into the immediate category of depression,” Esparza said. “The grieving process has to be
addressed.”
“We just happen to live in a grief-deprived society,” Coalson explained. “No one listens to you; they just
want you to say you are OK. You look fine, why aren’t you fun anymore. … You need to build and create
a new support system. And allow time to grieve.”
“You have to accept that you are already different,” she continued. “There are stages of grief. Getting
grief education can help you feel calmer. And you should not try to rush it. It’s a discovery process.”
“And you just might discover a new life purpose and/or career path that you would not have taken if you
didn’t address the changes in your life after a TBI. Another positive from grieving is that when you are
triggered, say a year from now, it will not be as intense of an emotion and you will move along,” Coalson
said.
Kocina stressed the necessity of quality sleep in your physical and mental recovery process. She also
explained the energy Reserve Model. (Link to attachment.)
“It’s more difficult to deal with grief and trauma when you are not sleeping well,” Kocina explained. “If
you can take care of your sleep, you can take care of this injury better.”
Along with grief and sleep deprivation there is this “disbelief” about the injury.
“What is the emotional injury of the TBI?” Esparza said. “You have to get to the core of who you are and
eventually you will have to ask this question: What is the meaning of this injury in my life? How are you
going to adapt to this change in life? What we do know is that life continues in this riptide of change. In
the midst of the most terrible circumstances what is the next step? It doesn’t have to be catastrophic.”
Stone stressed that psychologists “don’t have a magic wand, but it’s inspiring” to work with members of
the TBI community. “It’s an incredible privilege to be on this journey with you.”
“We are here to support you,” Kocina said. “Let the therapist know what you need and tell them what is
not working. You are not going crazy. You are the same person, but your future looks different.”
Coalson noted: “It’s an ongoing journey. Do the self-care. Don’t’ fight yourself. You can like yourself,
even if you don’t like what is going on.”
CTAT, LLC
6732 West Coal Mine Avenue, Suite 227
Littleton, CO 80123
© 2025 CTAT, LLC
